The Ontario Chief Coroner's reports are clear — alarm about MAID in Canada isn't warranted
A guest article by James Downar and Jocelyn Downie

In October, the Office of the Chief Coroner for Ontario (OCC) released three reports on medical assistance in dying (MAID) cases from last year. These reports have generated significant commentary, including the claim that MAID is being disproportionately accessed by marginalized people. I did a brief assessment of these claims here. In the following article—the first ever guest post for Value Judgments!—James Downar and Jocelyn Downie discuss the data much more thoroughly. The reports themselves were sent to some physicians by the OCC, but haven’t been easily available to the public. I’ve included the files at the end of the article. –Eric
Summary
The Office of the Chief Coroner (OCC) of Ontario recently released three reports about recipients of Medical Assistance in Dying (MAID) in that province. The reports have been the subject of a number of false or misleading claims suggesting that Ontarians had received MAID because of difficulty accessing housing, or due to social distress or untreated mental illness. In fact, the reports suggest the opposite.
The reports included a large amount of data about MAID recipients—data that dispel the concern that MAID might disproportionately affect the vulnerable or marginalized:
While MAID cases continue to rise, MAID cases for people whose natural deaths are not foreseeable (Track 2) actually fell in 2023, and remains extremely rare (0.09 percent of deaths)
95 percent of those in Track 2 with a self-reported disability received supportive services.
Only four (3 percent) Track 2 recipients had previously been found ineligible for MAID, and there is no evidence that “doctor shopping” lay behind these cases (as opposed to, for example, a change in the person’s condition).
The prevalence of isolation or self-perceived burden among MAID recipients is either the same or lower than the prevalence of these reports in community-dwelling or terminally ill people who do not seek MAID, suggesting that these factors are not driving MAID to any substantial degree.
Men are more likely than women to receive MAID overall. More women receive Track 2 MAID, but this observation is limited to specific conditions that are known to be much more common in women than men. For other conditions, the gender split in Track 2 MAID follows the known gender differences in disease prevalence—sometimes equal between men and women, and sometimes more in men. This suggests that observed gender differences in MAID recipients simply reflect gender differences in disease.
MAID recipients are much more likely to live in private residences, and less likely to be in residential care/long-term care than those who die naturally. Many older MAID recipients live alone, but at rates that are very similar to the population average for their age, again suggesting that this is not a factor driving MAID.
MAID recipients are less marginalized/more privileged than the average dying Ontarian who is categorized as “palliative”.
MAID recipients with self-reported disabilities are overall slightly less marginalized/more privileged than the average dying Ontarian who is categorized as “palliative”, and less marginalized/more privileged than the average Ontarian living with a neurodegenerative disease.
Track 2 recipients overall are approximately as privileged/marginalized as the average dying Ontarian who is categorized as “palliative” or the average Ontarian living with a neurodegenerative disease.
Previous reports that Track 2 MAID recipients are more marginalized than the average Ontarian are misleading because people who die without MAID, or people living with chronic illness show exactly the same degree of marginalization. This is because the marginalization index includes factors more common among seniors. If marginalization is associated equally with the decision to receive MAID as it is associated with the decision not to receive MAID, then we must accept that these findings simply reflect factors associated with disease and age, not the decision to pursue MAID.
The reports also include summaries of six cases (three for mental illness, three for social distress) that were selected for their complexity and ability to generate discussion, acknowledging that “only a small number of MAID deaths in Ontario have identified concerns.”
The case reviews were used to generate recommendations for MAID practice and oversight, not to determine wrongdoing or establish that a person had received MAID for any reason other than what was intended in the law. MDRC members who publicly reference their own comments in the report as “findings” are being disingenuous.
Psychiatrists were heavily involved in the care of all three cases where mental illness was a consideration. In two cases, the MDRC found that the psychiatrist was “beneficial” or “instrumental” in establishing that the MAID request was not the result of untreated mental illness. In the third, the patient was admitted under the care of a psychiatrist, but the psychiatrist was not one of the MAID assessors. Still, the MDRC clearly did not conclude that the MAID request was caused by untreated mental illness.
For the cases in which social distress was a consideration, all three had been offered (and generally accepted) substantial social support but continued to experience distress and requested MAID in spite of this. Housing was mentioned as a consideration in only one case, and the majority of the MDRC correctly concluded that “other housing arrangements would not have led to the resolution of her suffering.” To be clear, the committee did not conclude in any case that the MAID request was the result of social distress.
Introduction
The Office of the Chief Coroner (OCC) of Ontario recently released three reports about recipients of Medical Assistance in Dying (MAID) in Ontario.1 The reports have been the subject of a number of false or misleading claims in Canadian and international media, as well as on social media websites.2 It has been suggested that Ontarians have received MAID because of difficulty accessing housing or due to social distress or untreated mental illness. In fact, the reports suggest the opposite. It is important to understand what is really in these reports as well as how to interpret epidemiologic data about the recipients of MAID, in order to have a clear understanding of what actually appears to be driving (and what is not driving) the practice of MAID. Of course, data does not answer moral questions, and people may be opposed to MAID for any number of reasons, but this does not justify anyone misrepresenting data.
The three reports are:
Complex Medical Conditions with Non-Reasonably Foreseeable Natural Deaths
Navigating Vulnerability in Non-Reasonably Foreseeable Natural Deaths
Medical Assistance in Dying (MAID): Marginalization Data Perspectives
The first two reports each include a set of data collected about MAID recipients, followed by a description of three cases, with an overview of the MDRC’s discussion about each case. These reports conclude with a list of recommendations for different organizations. The third report, issued by the Office of the Chief Coroner, specifically focuses on additional data related to marginalization.
In this paper, we will first explain the purpose, composition, and process of the Committee that prepared the reports. We will then present and discuss the data presented and the cases reviewed. There may be important insights to be drawn from the reports—but they are not those the anti-MAID activists and journalists misrepresenting the reports would have the public and policymakers believe.
The MAID Death Review Committee (MDRC)
The MAID Death Review Committee (MDRC) was created in January 2023 by the Office of the Chief Coroner of Ontario (OCC). The purpose of the MDRC is to:
…review relevant MAID trends, topics, or issues and offer insights, perspectives, or interpretations and assist in formulating recommendations to inform system improvements (e.g., education of MAID practitioners, review of regulatory body policies) with a goal to support quality practice and the safety of patients and MAID practitioners.3
The MDRC is a multidisciplinary committee with sixteen members who include a range of perspectives on MAID itself, including individuals who have been longstanding opponents of MAID as well as MAID assessors and providers. The reports make it clear that the MDRC was not intended to judge individual cases, and it does not have the mandate or capacity to issue findings about what motivated a particular MAID request nor to judge whether assessors and providers acted inappropriately or not in accordance with the law.
The reports also make it clear that the Committee “did not aim to establish consensus.”4 The reports include a summary of the case discussions by committee members, and hence include some comments articulating a negative interpretation of events. But this does not mean that these negative interpretations are established facts. MDRC members who have publicly referenced their own comments in the reports as findings are misrepresenting the reports.
The MDRC reviewed the data collected by the OCC. They were also provided with “MAID deaths illustrative of specific circumstances, identified during review by the MRT.” They then produced the two Committee reports referenced above to fulfil their purpose.
The Data
How to draw accurate insights from the data
The data gathered by the OCC and reviewed by the MDRC included information about the illnesses, suffering, and demographics of those receiving MAID. This information can be helpful for learning about the people applying for MAID, and might offer insight into why they are seeking MAID. However, if you want to gain accurate insights into the practice of MAID itself, you must always compare MAID recipients to an appropriate comparator group: people with similar conditions (i.e., terminal or chronic illness) who are not asking for MAID.
This is done to avoid a “cohort effect”, which is well known in research.5 For example, if you study a group of people who are all followed by a cardiologist, it is very likely that these people will have a higher risk of mortality than the general population. This is not because cardiologists are dangerous, but because they follow people with heart disease, which carries an elevated risk of mortality. To better understand the association between cardiologists and mortality, you would need to control for this confounding effect6 by looking exclusively at people with heart disease (for example), and compare those who are followed by cardiologists to those who aren’t. In MAID recipients, you expect a certain degree of marginalization (e.g., higher age, lower socioeconomic status) compared to the population average due simply to the fact that terminally or chronically ill individuals are older than the average person, and chronic illness has a negative impact on socioeconomic status. If you want to understand specifically the degree of marginalization associated with MAID, you need to look for the degree of marginalization in MAID recipients relative to those with terminal and chronic illnesses who are not seeking MAID. Likewise, for other measures of patient experience or suffering (e.g., loneliness, self-perceived burden), you must always know about the experience or suffering of those who are not seeking MAID, to avoid mistakenly assuming that these factors are driving the practice of MAID.
Of course, we are not saying that we don’t or shouldn’t care about these forms of marginalization or suffering, or that they do not cause harm and death in society. On the contrary, we know that income inequality alone is associated with tens of thousands of deaths annually.7 But if we see that MAID recipients are equally or less marginalized than people with terminal or chronic illness, then we know that the link between marginalization and death is not through MAID but through the conditions that make people eligible for MAID in the first place. We cannot mitigate the effects of marginalization through MAID eligibility, but rather through better policy aimed at addressing the social determinants of health.
What does the data show?
There was a lot of data included in the reports. In this section, given the focus of the false and misleading claims made about the reports and MAID in Ontario, we present the data that is most relevant to the questions of what is driving people to request MAID and whether there are any good reasons to be concerned about the practice of MAID in Ontario.
Numbers of Cases
The total number of MAID cases continues to increase: 4528 in 2023 vs. 3813 in 2022. Notably, this increase was exclusively among Track 1 MAID recipients.8 Cases among Track 2 recipients decreased to 116 in 2023 from 121 in 2022. The relative proportion of Track 2 cases thus decreased to only 2.5 percent of all MAID cases.
Illness, Disability and Supports
The underlying illnesses for MAID recipients was largely in line with previous federal reports.9 Most had cancer (61 percent), followed by cardiovascular (19 percent), respiratory (15 percent), and neurological disease (13 percent). Among Track 2 recipients, the most common condition was chronic pain (40 percent), followed by neurodegenerative illness (38 percent), “other” (34 percent), and frailty (24 percent). Many Track 2 recipients had more than one condition.
In terms of disability, 24 percent of Track 1 recipients and 63 percent of Track 2 recipients self-reported a disability, as compared to 27 percent of the general population. The discrepancy between tracks is not surprising, given that Track 2 recipients generally have longstanding conditions that cause functional impairment while Track 1 recipients often have more acute declines, meaning that people might not self-identify as having a disability. In 85 percent of cases in each track, the disability was mobility related, but we do not know the severity of the disability. Reassuringly, 95 percent of those with a self-reported disability were receiving supportive services. The reports do not include data indicating that these services were in any way inadequate.
“Doctor Shopping”
Some commentators have expressed concern that MAID applicants may pursue an unlimited number of assessments until they find two assessors who find them eligible. This is commonly and pejoratively referred to as “doctor shopping”. Among those receiving Track 1 MAID, 13 (0.3 percent) had previously been found ineligible for MAID at some point. For Track 2 MAID recipients, four (3 percent) had been previously found ineligible. These numbers are very small, and it must be understood that there are legitimate reasons why someone can be found ineligible on one assessment, but eligible on another. For example, Track 1 patients with advanced cancer can be delirious due to a reversible cause (e.g., infection, opioid toxicity), prompting one assessor to correctly indicate that they are not capable of consenting to MAID, while, after reversal of the delirium, a subsequent assessor would correctly find that they were now capable of consenting to MAID. Track 2 recipients on their initial assessment may not have been informed about and given serious consideration to the means available to relieve their suffering, prompting an assessment of ineligibility. However, if they went on to receive the information and give serious consideration to these means, they could then be deemed eligible. Since the details of the previous findings of ineligibility, and the reasons for the current finding of eligibility, are not provided in the reports, the data cannot be taken as evidence of “doctor shopping”.
Type of suffering and relief offered
MAID recipients were able to indicate the type of suffering that they were experiencing and could indicate more than one type. As has been the case in every report in every jurisdiction where MAID is legal, the most common type of suffering was the loss of ability to engage in meaningful activities (96 and 97 percent), and loss of independence (87 percent and 82 percent) for Track 1 and Track 2, respectively.
Isolation or loneliness was reported by 16 percent of Track 1 and 40 percent of Track 2. According to StatsCan,19–24 percent of seniors feel isolated and wish they could participate in more social activities.10 This increases with age and chronic health problems, meaning that these are very similar to what you would see among similar people who are not requesting MAID. Seniors are an appropriate comparator group here, since 85 percent of Track 1 and 75 percent of Track 2 recipients are 65 years old or older.
Self-perceived burden on family, friends or caregivers was reported by 43 percent of Track 1 and 39 percent of Track 2 recipients. However, studies of people with advanced cancer and Amyotrophic Lateral Sclerosis (ALS, a degenerative neurological condition) who are not pursuing assisted death often report a much higher prevalence of self-perceived burden (up to 73 percent11), suggesting this is also a cohort effect related to serious illness rather than a specific driver of MAID. Note also that the concept of “self-perceived burden” is well-known in studies of people with advanced illness and represents an important component of existential distress—a form of distress that is very difficult to treat, and that is the main reason people request MAID. Self-perceived burden is very different from the idea that others are making the person feel like a burden.
The most common means of relieving suffering in Track 2 was pharmacological (90 percent), with mental health and disability supports offered in 41 percent of cases. Community services, including housing and income support, were offered to a low proportion of persons (under 10 percent). However, there is no evidence in the reports that any MAID recipients required such supports. Financial or housing concerns were not listed as a cause of suffering for any MAID recipient in the reports (there is an “Other” option on the data collection form, but apparently it was not selected for any MAID recipient in either track). The question of housing is further explored in the cases below.
Navigating the MAID process
Under the law, for Track 2 patients, there must be a clear 90 days between the beginning of the first assessment to the provision of MAID unless there is an identified risk of imminent loss of capacity (in which case it is any shorter time period considered appropriate by both assessors). In total, 42 percent of Track 2 MAID recipients took more than 120 days from the beginning of the first assessment to the provision of MAID. Twenty-four percent took more than six months and 13 percent took fewer than 90 days. For these 13 percent, it is not clear whether (1) this was the result of an honest misunderstanding about precisely when the required 90-day period begins; (2) there was an identified risk of imminent loss of capacity (and therefore shortening of the 90-day requirement); or (3) there was a switch to Track 1 due to a change in condition (which also removes the 90-day requirement). It is therefore not valid to draw the conclusion that the law was not respected from the data provided in the reports.
In 1.7 percent of Track 2 (two cases), no experts in the field were consulted. However, while this is a legislated requirement for Track 2, the initial assessor may have had the required expertise, or the applicant may have had a condition for which there is no recognized expert (e.g., long COVID). It is not clear from the reports whether this was the case in the two cases.
Demographic Data
Among Track 1 MAID recipients, men appear to have a 20–40 percent higher incidence of MAID across all age groups. Among Track 2 recipients, the rate of MAID is 20–50 percent higher in women across all age groups. The federal reports of Track 2 MAID show that the gender split varies substantially according to the medical condition prompting the request (See Chart below).

Track 2 MAID recipients for neurological conditions (the most common category for Track 2 MAID) were actually more likely to be men. This makes sense if you know that Parkinson’s Disease (the most common condition in this category) occurs in men almost twice as often as women.12 In contrast, Track 2 MAID recipients for “multiple comorbidities” (e.g., frailty conditions) and “other” (e.g., chronic pain) were more likely to be women. This makes sense if you know that frailty is almost twice as common among women as it is among men13, and chronic pain is also more common among women.14 The remainder of Track 2 conditions show no sex difference, consistent with the fact that the age-adjusted incidence of these conditions (postmenopausal cardiovascular disease,15 respiratory disease,16 cancer,17 etc.) is similar between sexes. In other words, the sex differences observed in Track 2 MAID recipients are easily explained by the sex differences in the conditions that are prompting MAID requests, not any gender bias against or risk of abuse for women. It is unreasonable to justify a selective concern about female predominance in a subset of Track 2 cases, when there is either no gender split (or male predominance) for every other condition in Track 2, and a male predominance in Track 1 (which is 50 times more common than Track 2).
Living Situations
The vast majority of MAID recipients live in private residences (91 percent of Track 1 and 84.5 percent of Track 2). A small proportion live in residential care/long-term care (five percent of Track 1, 11 percent of Track 2), which is much lower than the average among Ontario decedents (around 25 percent).18 Interestingly, around three percent of recipients on both Tracks 1 and 2 were in palliative care facilities.
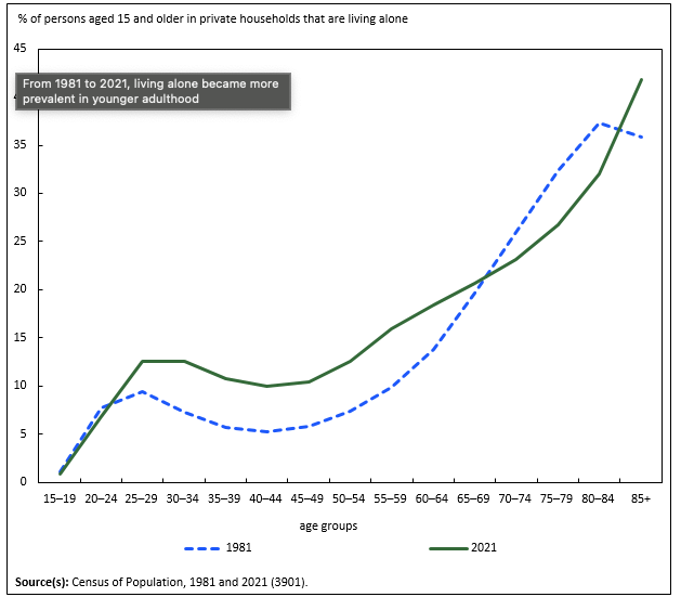
A fair proportion of MAID recipients live alone, but at every age group, the number is very close to the population average (see Graph below from Statistics Canada). Exceptions would be those 90 years old and older; StatsCan only measured up to 85 and older, but it seems likely that Track 2 recipients over age 90 (73 percent) were slightly more than the population average (probably over 50 percent) albeit with very small numbers. Track 2 recipients were less likely to have an immediate family member as their next of kin (73 percent vs 90 percent). No reliable comparator for Canada was provided in the reports, so conclusions of increased vulnerability cannot be drawn on the basis of the data presented.
Marginalization Indices
The Ontario Marginalization Indices were developed to quantify different dimensions of marginalization. There are four indices (descriptions from the PHO website19):
Material Resources: Closely connected to poverty and refers to the inability for individuals and communities to access and attain basic material needs relating to housing, food, clothing, and education.
Racialized and Newcomer Populations: The proportion of newcomers, and/or non-white, non-Indigenous populations.
Households and Dwellings: Family and neighbourhood stability and cohesiveness, and is based on measures of the types and density of residential accommodations and family structure characteristics. Note that this does NOT refer to the quality of housing.
Age and Labour Force: Area-level concentrations of people who don’t have income from employment, including older adults, children, and/or those unable to work due to disability.
From the above descriptions, it is clear that some indices are more helpful than others for identifying those who might be structurally vulnerable in a way that is relevant to MAID and end-of-life care. Material Resources and Racialized and Newcomers would be potentially helpful. Households and Dwellings, and Age and Labour Force are unhelpful for identifying vulnerability populations that are mostly elderly, and those with chronic illnesses that preclude them from working. Marginalization indices are generated from area-level average metrics based on postal code, which has been validated as a reflection of individuals. However, the fact that each index has multiple different factors, and there is variability within a postal code area, further underscores the need to compare MAID recipients to appropriate comparator groups.
One can compare marginalization quintiles in many ways. One approach is to compare the total proportion in the two most marginalized quintiles (Q4/5), and the other is to compare the difference between the proportion in Q5 (most deprived) and Q1 (least deprived; Q5 –Q1). In both cases, higher numbers suggest more marginalization.
MAID recipients are less marginalized/more privileged than the average dying Ontarian who is categorized as “palliative”. This is shown both in the percent in the two most marginalized quintiles (Q4/5; 41.8 percent in MAID, 45.5 percent in all decedents) or by measuring the difference between the percent in the most and least marginalized quintiles (Q5 – Q1;1.2 percent in MAID, 8.4 percent in all decedents). This echoes previous studies from Ontario showing exactly the same finding with income.20 (Material resources are related to income but include other considerations.) The numbers in the MRDC reports are similar to data in those studies, suggesting that this observation is stable over time.
MAID recipients with self-reported disabilities are overall slightly less marginalized/more privileged than the average dying Ontarian who is categorized as “palliative”, and less marginalized/more privileged than the average Ontarian living with a neurodegenerative disease. Depending on the duration of the disability, the Q4/5 totals for MAID recipients range from 40.3 to47. 1percent, compared to 45.5 percent for all decedents and 46.5 percent for those with neurodegenerative disease. The Q5 – Q1 measures for MAID recipients range from –0.8 to +8.1 percent, compared with 8.5 percent in all decedents and 9.1 percent in Ontarians living with neurodegenerative disease.
MAID recipients with disabilities for seven months to four years were less marginalized/more privileged than all decedents or Ontarians living with a neurodegenerative disease. MAID recipients with a disability for less than six months or more than four years were as privileged/marginalized as the average decedent or the average Ontarian with a neurodegenerative disease.
Track 2 recipients overall are approximately as privileged/marginalized as the average dying Ontarian who is categorized as “palliative” or the average Ontarian living with a neurodegenerative disease. Those who had their condition for fewer than 10 years were slightly more privileged than the average Ontarian decedent or person living with a neurodegenerative condition; those who had their condition for more than 10 years were slightly more materially deprived than the comparator group. The data from the Track 2 columns above can be combined through simple multiplication, indicating that the total Q4/5 is 49.9 percent (compared with 45.5 percent for all decedents and 46.5 percent for those with neurodegenerative disease) while the Q5 – Q1 measure for Track 2 MAID is 9.5 percent (compared with 8.5 percent in all decedents and 9.1 percent in Ontarians living with neurodegenerative disease). It must be emphasized here that Track 2 numbers are very small. The total for 2023 (116) decreased from the previous year (120). One more or one fewer case would change these comparisons.
Track 1 recipients show the opposite trend. Those who had their illness for fewer than 10 years (Q4/5= 39.1 percent, Q5 – Q1= –0.7 percent) were more privileged than those who had their illness more than 10 years (Q4/5 = 41.9 percent, Q5 – Q1 = 1.1 percent)
The other marginalization indices presented in the reports revealed data that was expected or is not instructive. For example, racialized and newcomer populations have very low involvement in MAID regardless of Track (Q5 – Q1= –15 percent and –19 percent, respectively), but no comparators were provided. Unpublished data from 2010–2019 showed a Q5 – Q1 of –4.7 percent. Racialized and newcomer populations are well known to be less involved in MAID, and more likely to receive aggressive care (including ICU) at the end of life.21 For the reasons explained above, the housing and labour force indices are not indicators of marginalization in end-of-life populations or seniors in general (who account for over 80 percent of MAID).
Notably, one MAID opponent responded to the reports by highlighting the fact that many MAID recipients were in the highest quintile for “housing instability”.22 However, the author clearly misunderstood the housing and dwelling index, which reflects the proportion of residents who stay long-term in a neighbourhood, live alone, and are single, divorced, or widowed, among other factors. The cost of housing, for instance, isn’t included. Any neighbourhood with many seniors would show higher turnover, including some of the wealthiest neighbourhoods in Canada (e.g., Toronto’s Yorkville neighbourhood23), as was pointed out in the report. For populations known to be elderly with chronic or terminal illness, this index does not reflect vulnerability at all.
Case Reviews
The first two MCRC reports each included three cases that were meant to illustrate dimensions of complexity.
Cases in which Mental Illness was a Consideration
There were three cases in which, the reports claim, mental illness was a consideration. It must be noted that, under current Canadian law (until March 2027), a “mental illness” cannot be considered a “serious and incurable illness, disease, or disability” and so a person with a “mental illness” as their sole underlying medical condition cannot be eligible for MAID. These are all, therefore, cases in which mental illness is present but is not the patient’s sole underlying medical condition.
Furthermore, not one of the cases is an example of someone receiving MAID for mental illness reasons, and mental illness was probably not even a factor in Case C.
Case A: A man in his forties had multiple forms of suffering (apparently including pain) and severe functional decline post-vaccination for COVID. There was no unifying diagnosis, but he had a history mental illness (depression and possibly trauma). He was admitted for inpatient psychiatric care for suicidal ideation/PTSD. The case report suggested that these were being managed at the time of the assessment, although the psychiatrist was not one of his MAID assessors. His MAID assessors found him eligible, with the diagnosis of likely myalgic encephalomyelitis. Ultimately, no pathology was identified on autopsy.
Case B: A man had longstanding gastric and duodenal ulcers causing pain. He also had a history of mental illness, including depression, anxiety, narcissistic personality disorder, and bipolar disorder type 2. He had made a prior suicide attempt about one year previously (a fall from height), which left him with extensive injuries and functional decline despite a prolonged rehabilitation course. A psychiatrist determined that neither psychiatric illness nor suicidal ideations were prompting the request for MAID.
Case C: A man in his eighties had chronic pain and adjustment disorder due to a 15-year history of spinal stenosis/adhesive arachnoiditis. He was followed by a pain specialist. He had been diagnosed by a psychiatrist with adjustment disorder “influenced by irremediable chronic pain, and less likely to be responsive to pharmacologic intervention.” The patient declined further treatment, and this was considered to be an informed decision by the psychiatrist.
The Committee report highlighted some themes emerging from these cases:
Uncertain diagnosis
It should also be noted that diagnostic certainty is not the standard required by law. Rather, the law requires that both assessors “be of the opinion” that the person meets all the eligibility criteria, one of which relates to diagnosis (i.e., “serious and incurable illness, disease, or disability”).
Ultimately, MDRC members accepted that diagnostic certainty is not always feasible. In palliative care, people are sometimes admitted for end-of-life comfort care even when there is no certain diagnosis, but just a clear notion that whatever the person has, there is no realistic prospect for improvement, and the person’s goals of care are focused on comfort.
…diagnostic certainty is not always feasible due to the imperfect nature of clinical knowledge and evaluation, the overlap between psychological and physical somatic clinical presentations, and a reliance on diagnosis by exclusion.24
There were suggestions in the MDRC report that assessors should ensure a well-documented and comprehensive clinical evaluation and investigation of an uncertain diagnosis by multiple specialists. Some suggested consulting multiple specialists and “different treatment modalities trialed, spanning different functional orientations of the illness presentation, and addressing all probable conditions”. But, and this warrants emphasis, there was no conclusion that the medical teams failed to do this in any of these cases.
Concomitant psychological disorders
The MDRC report was quite clear that in each case, involvement of psychiatric expertise was good: “All of the requestors in the deaths reviewed benefitted from a psychiatry referral.”
The most critical comment in the report was fairly muted and applied to only one case: “In Case A, the role of psychiatry was potentially underutilized for the purposes of MAID eligibility determinations.” Case A was a patient admitted under the care of a psychiatrist, so the MDRC seems to have hoped that the psychiatrist would have been one of the assessors. There was no indication that the psychiatrist disagreed with the finding of capacity made by the MAID assessors, but some MDRC members felt the duration of the physical condition could have been longer to ensure irremediability. More time may have provided a greater degree of certainty around irremediability, but this must be balanced with the additional suffering experienced by the person with the condition as they waited. Notably, no specific duration was indicated by the MDRC members who suggested more time, and, of course, any duration would be arbitrary. Also, as indicated previously, certainty is not the standard required by law.
In the other cases, the reports highlighted how helpful the psychiatrists had been for clarifying that the person requesting MAID was competent and eligible for MAID:
In Case B, psychiatry was consulted to differentiate suicidal ideations from a MAID request and to evaluate decisional capacity to engage in the MAID process. This consultation process was identified as a beneficial approach to practice by multiple members.25
In Case C, psychiatry’s role was instrumental in identifying that the diagnosed adjustment disorder was not reversible or treatable due to the nature of the stressor (i.e., severe, and refractory chronic pain).26
Beyond medical records
The MDRC highlighted the importance of multidisciplinary care and potentially involving the family in discussions, not just relying on medical records. However, there was no indication/suggestion that the medical team failed to engage with the existing care team and family. While looking beyond medical records seems a sensible recommendation, there is no evidence in the report that the medical team failed to do this in any case.
In sum, it is not clear that any of the cases presented were examples of an ineligible person receiving MAID. In all three cases, the person was under the care of a psychiatrist, and in two of the three cases, the psychiatrist’s assessment was critical to establishing that the person had decision-making capacity and that the psychiatric condition was not driving the MAID request. In the third case, there was a narrow, implied criticism that, although there was a psychiatrist treating the person who apparently didn’t disagree with the plan for MAID, this person should have been specifically involved as a MAID assessor. The diagnosis was believed to be physical, not psychiatric, and there seemed to be a general belief that this was a reasonable judgment. One might disagree with these individuals’ decisions to request MAID, but not one of these cases is an example of someone receiving MAID for psychiatric reasons, and psychiatric illness was probably not even a factor in Case C.
Cases in which social deprivation or other forms of marginalization were a consideration
There were three cases in which social deprivation or other forms of marginalization were a consideration.
Mr. A: A man in his forties had Inflammatory Bowel Disease that was severe enough that it had affected his ability to work or form a social network. He had received “extensive treatment.” He was dependent on family for housing and financial support. He “had declined multiple social support programs and psychosocial services.”
Mr. A had a history of mental illness and substance use disorder. Some MDRC members felt that “his substance use was not explored in the MAID assessments, and he was not offered addiction treatments.” Some MDRC members were concerned that evaluations only had “limited exploration of medical and social issues experienced by Mr. A” and that “Mr. A’s mental illness was not fully examined for remediation.” However, given that the psychiatrist had a longstanding relationship with the patient, it is likely that these issues had been explored previously by the psychiatrist, and that the MAID documentation simply did not include these explorations.
Mr. A’s treating psychiatrist had raised the option of MAID (and ultimately transported him to his MAID procedure). This clearly generated conflicting views on the MDRC:
A few members discussed that bringing forward MAID in this context may undermine a person’s resilience and confirm an impression that their life is not worth living. MDRC members with both psychiatric and MAID expertise provided another view. These members identified that discussions of MAID can be clinically informed and well-timed when fully considering a person’s treatment history and suffering, albeit respecting continual professional guidance on this issue.
The report included the statement that “[p]ausing MAID assessments and facilitating measures and interventions to reduce social isolation may have been a valuable and beneficial approach when seeking options to alleviate suffering for this person.” While this is a true statement, the report also made clear that the patient had been offered and refused these in the past, and that his request was prompted by his Inflammatory Bowel Disease (a physical ailment).
The MDRC report also included comments about encouraging family engagement. However, the case description did not suggest that poor family engagement was an issue.
Ultimately, this was a person with a clear underlying, debilitating medical condition, apparent family support, and psychiatric supports being provided. People might disagree with his decision and be concerned that the possibility of MAID was raised by a healthcare provider, but the patient clearly had access to all manner of psychosocial supports. A psychiatrist raising MAID in a case in which a person might be eligible does not violate regulatory policies or standards.
Ms. B: A woman in her fifties had multiple chemical sensitivity syndrome (MCSS). This case appears to be a well-known case (“Sophia”), which had already been discussed in some detail in the media, but now more case details were available including that “[s]he had a history of psychiatric hospital care for depression, anxiety, suicidality, and post-traumatic stress disorder, related to childhood trauma.”
Ms. B had trouble securing housing to meet her needs due to MCSS. After a lengthy delay, she ultimately secured funds for renovation after she won a ruling from the Human Rights Tribunal. The renovations “did not satisfactorily address her MCSS symptoms”, so her condition worsened. According to the description,
A remaining option presented was to live in a small hypoallergenic space (i.e., a bubble). As a result of her housing situation and conditions, necessary to address her MCSS, Ms. B experienced social isolation, which greatly contributed to her suffering and request for MAID.
To be clear, Ms. B’s initial struggle to get appropriate housing was a failure of social supports. But her subsequent isolation and resulting suffering was brought on directly by her medical condition, not a failure of social supports. Ms. B’s situation is analogous to people with fragile immune systems who have to self-isolate to protect themselves from infection.
The discussion in the report suggests that some MDRC members questioned the existence of MCSS and believed that Ms. B was suffering from a somatic symptom disorder, but no supporting information was provided for this belief.
Some MDRC members suggested “there were other housing options to explore (e.g., a small trailer in a more rural setting).” However, this was a woman with an advanced medical illness who required a motorized scooter to mobilize. It is absurd to suggest that such a person would improve their social isolation by moving out to a rural area, hours from family, and live by herself in a trailer. The report ultimately indicated that “[m]ost MDRC members believed that Ms. B’s MCSS presentation required her to continue living in isolation in a small hypoallergenic environment and hypothesized that other housing arrangements would not have led to the resolution of her suffering.” Ms. B herself made this same point in a letter to Dr. Chantal Perrot (made public after her death).27[27]
Mr. C: A man in his forties had quadriplegia following a motor vehicle collision more than two years prior to his request for MAID. He had been isolated during the COVID pandemic. Rehabilitation produced no “physical or functional gains”. Returning home was “not feasible” given the degree of his supportive needs. He was a member of a racialized and religious community. He was very distressed about his ability to maintain a relationship with his young children in view of his medical condition.
This case started as Track 2, but one assessor indicated that he could become Track 1 if he developed septicemia that would then be untreated. This was flagged as potential “track switching” by some MDRC members, as if there was something nefarious afoot. However, untreated sepsis is clearly a risk for people with quadriplegia and, untreated, would constitute a reasonably foreseeable death (the criterion for being on Track 1). This is entirely consistent with the law.
Some MDRC members were concerned about the duration of disability and felt that the patient was still in “transition”. Others felt that one assessor did not have a “purposeful approach for navigating expertise and offering care options.” Some members expressed concern that the assessors did not engage psychiatry or rehabilitation services. However, he had already gone through rehabilitation without benefit. Some suggested “peer mentoring”, psychosocial guidance for navigating relationships with children, and “social solutions for enhanced community and cultural engagement.” These might have been helpful, although no evidence was presented in the report that they were not offered. There was also concern expressed about “relational conflict” and the potential impact of that on his suffering.
Ultimately, while many people might not choose to proceed with MAID in this context, this does not seem to have been an impulsive request by someone suddenly faced with a transition. The request was made over a year (perhaps almost two years) since the injury, with no functional recovery. The patient could have received some of these other forms of social supports, but he also had the right to privacy if he chose not to get these supports or to engage his ethno-religious community for fear of judgment. The reports also include no clear evidence that these approaches are routinely effective (or that they are effective at all). There are always a range of options that could be considered for complex cases, but there was no evidence presented in the report of any lapse in care standards in this case.
It is not clear that any of the cases presented in the report were clear examples of how social interventions, services, etc. would have addressed the suffering and changed the request for MAID. Mr. A had received (and refused) a great deal of support. Ms. B’s only other option was to seek out isolation to control her medical condition. Mr. C had experienced a devastating injury and had waited almost two years, failing rehabilitation etc. before requesting MAID. His distress may have been lessened by engagement of family/religious group, but it could just as easily have worsened as a result. We may disagree with their decisions to request MAID, but not one of these cases is an example of someone requesting MAID for purely social distress, and social distress was arguably not even a factor in Ms. B’s MAID request.
Conclusion
The MDRC and OCC reports are a helpful addition to our understanding of the practice of MAID in Canada. They present new data, reflections on case studies, and recommendations that should be carefully reviewed by all stakeholders. However, they have also been misunderstood and misrepresented. For example, early media stories suggested that these reports included evidence of social distress causing MAID requests, or a disproportionate involvement of the individuals struggling with material deprivation. The reports actually showed the opposite. We must be vigilant about how MAID is used, and aware of the potential for inappropriate use of MAID. We must also be vigilant against mis- and disinformation as that instills unjustified fear and lack of trust in the system and misleads policymakers both in Canada and abroad.
James Downar (dr.james.downar@gmail.com) is Head and Professor, Division of Palliative Care, Department of Medicine, at the University of Ottawa.
Jocelyn Downie (Jocelyn.Downie@dal.ca) is Professor Emerita in the Faculties of Law and Medicine at Dalhousie University.
MAID Death Review Committee (MDRC) Report 2024-2; MAID Death Review Committee (MDRC) Report 2024-3; and Medical Assistance in Dying (MAID): Marginalization Data Perspectives; published 2024 by The Office of the Chief Coroner of Ontario.
Gaind S. MAID and marginalized people: Coroner’s reports shed light on assisted death in Ontario. The Conversation (October 24, 2024).
Coelho R. Canadians with disabilities are dying needlessly. The Globe and Mail (October 28, 2024).
MAID Death Review Committee (MDRC) Report 2024-2. (p. 2).
MAID Death Review Committee (MDRC) Report 2024-3. (p. 3).
Miroshnychenko et al. Cohort studies investigating the effects of exposures: key principles that impact the credibility of the results. Eye 2022;36:905-6.
Miroshnychenko et al. Cohort studies investigating the effects of exposures: key principles that impact the credibility of the results. Eye 2022;36:905-6.
Tjepkema M et al. Cause-specific mortality by income adequacy in Canada: A 16-year follow-up study. (2014) Statistics Canada.
“Track 1” refers to the procedural safeguards that apply to individuals seeking MAID whose natural death has become reasonably foreseeable. “Track 2” refers to the procedural safeguards that apply to individuals whose natural death has not yet become reasonably foreseeable.
Fourth annual report on Medical Assistance in Dying in Canada 2022. Health Canada (2023).
Saji A, Oishi A, Harding R. Self-perceived Burden for People With Life- threatening Illness: A Qualitative Systematic Review. J Pain Symptom Manage. 2023 Mar;65(3):e207-e217. doi: 10.1016/j.jpainsymman.2022.10.016.
Bianco et al. Sex and Gender Differences in Neurodegenerative Diseases: Challenges for Therapeutic Opportunities. Int J Mol Sci. 2023 Mar 28;24(7):6354.
Collard et al. Prevalence of Frailty in Community-Dwelling Older Persons: A Systematic Review. J Am Geraitr Soc 2012;60:1487-92.
Blyth et al. Fact Sheet: Gender Differences in Chronic Pain Conditions. International Association for the Study of Pain. (June 2024).
Betai et al. Gender Disparities in Cardiovascular Disease and Their Management: A Review. Cureus 2024 May 5;16(5):e59663.
Chronic Obstructive Pulmonary Disease (COPD) in Canada. Health Canada Data Blog. Accessed on December 2, 2024 at https://health-infobase.canada.ca/datalab/copd-blog.html#did
Cancer statistics at a glance. Canadian Cancer Society. Accessed on December 2, 2024 at https://cancer.ca/en/research/cancer-statistics/cancer-statistics-at-a-glance#:~:text=Cancerpercent20incidencepercent20forpercent20malespercent20andpercent20femalespercent20inpercent20Canadapercent20inpercent202024&text=127percent2C100percent20malespercent20andpercent20120percent2C000percent20femalespercent20wouldpercent20bepercent20diagnosedpercent20withpercent20cancer
see Downar et al., CMAJ 2020.
Downar et al. CMAJ February 24, 2020 192 (8) E173-E181 (https://www.cmaj.ca/content/192/8/E173) and Redelmeier et al. BMJ Open 2021;11:e043547. (https://bmjopen.bmj.com/content/bmjopen/11/5/e043547.full.pdf)
Yarnell et al. JAMA 2017;318(15):1479-1488. doi: 10.1001/jama.2017.14418.
Gaind S. MAID and marginalized people: Coroner’s reports shed light on assisted death in Ontario. The Conversation (October 24, 2024).
MAID Death Review Committee (MDRC) Report 2024-2. (p. 14).
MAID Death Review Committee (MDRC) Report 2024-2. (p. 17).
MAID Death Review Committee (MDRC) Report 2024-2. (p. 17).
https://www.ourcommons.ca/Content/Committee/441/AMAD/Brief/BR11824538/br-external/PerrotChantal-e.pdf







Hey Eric there's just a small typo you should fix:
"Some members expressed concern that the assessors did not engage physiatry"
Otherwise good post. Thank you so much.
I would also like to see a policy that takes into account consultation with numerous Indigenous (First Nations, Métis and Inuit) communities so that their diversity of perspectives are represented.